By Noemia Siqueira, Helen Elsey, Jinshuo Li, Penelope A Phillips-Howard, Zahidul Quayyum, Eliud Kibuchi, Md Imran Hossain Mithu, Aishwarya Vidyasagaran, Varun Sai, Farzana Manzoor, Robinson Karuga, Abdul Awal, Ivy Chumo, Vinodkumar Rao, Blessing Mberu, John Smith, Samuel Saidu, Rachel Tolhurst, Sumit Mazumdar, Laura Rosu, Sureka Garimella
Marginalised urban residents living in slums and other areas of cities face difficulties in accessing healthcare. Frequently, the only healthcare available to these city dwellers are private or informal healthcare providers, where care comes at a high price and quality can be poor.
For low-income city residents, this can lead to people not seeking care due to the financial burden or being driven into deeper poverty to meet the costs of care. This can mean that their health conditions get worse and that they may be vulnerable to additional conditions, leading to spiralling poor health and poverty for the individual and members of their household.
In health economic language, vulnerable urban dwellers can face a severe economic burden when accessing healthcare. This burden can be translated into high out-of-pocket expenditures and a high percentage of catastrophic health expenditures (CHE), which happen when the patients’ healthcare spending exceeds a specified threshold from the household’s total income.
A group of ARISE researchers came together to investigate the economic burden of healthcare access for slum dwellers and other city residents in low- and middle-income countries (LMICs). To do this, we conducted a scoping review to find out information on this topic in existing literature.
We wanted to know how expenditure on healthcare differed among poor city dwellers and those living in slums in LMIC cities.
In this blog, we show the process of developing the scoping review and the main outcomes of this investigation.
A scoping review to produce evidence
A core activity of ARISE is to produce evidence that can be used to advocate for improvements in the health and wellbeing of marginalised urban residents in LMICs.
Scoping reviews have a great utility for synthesising research evidence and are often used to group existing literature in a given field. The University Libraries website states that “Scoping reviews are best designed when a body of literature has not yet been comprehensively reviewed or exhibits a large, complex, or heterogeneous nature not amenable to a more precise systematic review”.
Given the complexity and heterogeneity of the literature addressing the economic burden of healthcare access for marginalised urban populations, we agreed that a scoping review would be the appropriate approach to provide evidence on this theme.
The scoping process
We developed a collaborative review process with representatives from ARISE research partners in India, Bangladesh, Sierra Leone, Kenya and the UK. The review team had 21 collaborators from BRAC University in Bangladesh; LVCT Health and African Population and Health Research Center in Kenya; The Society for Promotion of Area Resource Centres and The George Institute for Global Health in India; the University of Sierra Leone in Sierra Leone; University of York, Liverpool School of Tropical Medicine, and the University of Glasgow in the UK.
The process aimed to strengthen research capacity which is one of the core elements of the ARISE Consortium’s work. Some members of the team had little experience with review design, so training at the Cochrane interactive learning platform was offered to provide concepts and methods applied in review studies. They were then able to put their learning into practice in the following review process.
To operationalise the review process, the review team was divided into three groups, core group: researchers with experience in conducting systematic reviews and/or data analysis; new reviewer group: junior researchers with little experience in review methods; and the advisory group: senior researchers with expertise in health economics or urban health. The core and new reviewer teams were responsible for developing all review activities, whilst the advisory team contributed to the interpretation of data.
In July 2020, we had a kick-off meeting to present and discuss the review protocol previously discussed with the review team. Before doing any systematic review of the literature, a detailed protocol that specified every step of the process was produced. In our second meeting, we discussed different review designs and the Cochrane course.
As our search of electronic academic databases retrieved many studies (N=5,673), the members of the core and new reviewer teams were reassigned into review sub-groups, each with three researchers including at least one member from the core team.
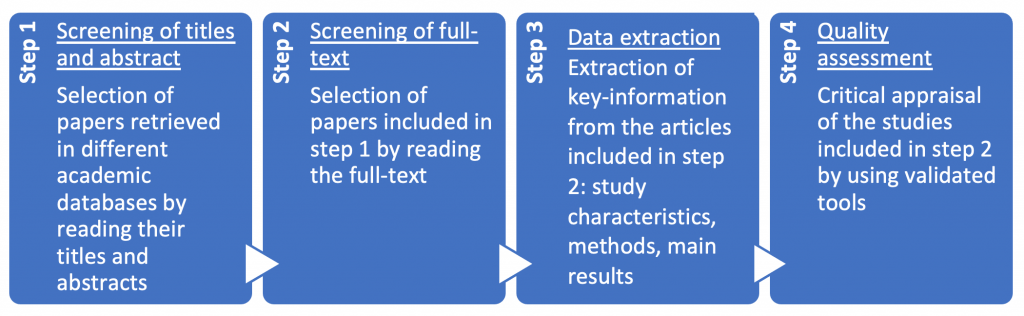
Each sub-group independently performed the review steps as illustrated in the flowchart below:
Disagreements arise in each step of the process over the inclusion or exclusion of studies, specific data extraction or scoring in the quality assessment of studies. To resolve the disagreements on steps 1 and 2, we had weekly meetings to debate each issue and reach consensus. Disagreements on steps 3 and 4 were resolved by the third reviewer of each sub-group.
Review outcomes
We classified the studies by their settings into:
- City-wide: urban studies which categorised residents by deprivation level but made no specific reference to whether people lived in slums or not
- Slum studies: urban studies with data collected only in slums, and
- Slum and non-slum: urban studies with data collected in slum and non-slum areas
We identified 64 studies for inclusion, 28 were from India, five from Bangladesh and one from Kenya. Our search did not identify any studies conducted in Sierra Leone.
The literature came mainly from city-wide studies, with 37 studies and a total sample of more than 1.5 million people. City-wide studies had more publications including the calculation of CHE, 20 in total. Unspecified and other health conditions (i.e. injuries, acute disease, child health and tuberculosis) were mainly addressed by city-wide studies, while slum studies addressed mainly obstetric and/or neonatal care. For chronic conditions, city-wide studies had more publications, but the total sample size was similar for city-wide and slum studies (~70,000 individuals).
Main findings
We found different expenditure patterns across the study groups. Slum studies reported higher direct costs of accessing healthcare for acute conditions than city-wide studies (Slum: ranged from I$157 poorest quintile to I$408 richest quintile; city-wide: ranged from I$125 poor quintile to I$177 richest quintile); and lower direct costs for chronic conditions (Slum: ranged from I$789 poorest quintile to I$1,695 richest quintile; city-wide: ranged from I$2,552 poorest quintile to I$3,166 richest quintile).
The percentage of individuals incurring CHE across wealth quintiles also differed according to the study group. By using a 10% threshold of the annual household income, we found similar percentages of CHE across wealth quintiles in slum studies (20% on average). However, in city-wide studies, the poorest residents incurred higher percentages of CHE compared with better-off residents (poorest quintile: 46%; richest quintile: 18%).
Process outputs and next steps
We published the review protocol in BMJ Open and the final manuscript has been submitted to the International Journal for Equity in Health.
We completed our scoping review in December 2021 after a huge effort from all team members. The commitment of the review team was crucial during this 1.5-year process as we had to deal with the tight agenda of the researchers and coordination across different time zones. The collaborative process was important to promoting a co-learning environment and a high-standard review.
Our next step is to translate the scientific findings into country-specific policy briefs with recommendations for action that are relevant to city and country contexts. We can then use the scoping review as a tool for advocacy and changes in policies to promote health and well-being for vulnerable urban residents.
Image credit: Kibera by Stefan Magdalinski is licensed by CC BY 2.0.